Understanding diabetes is crucial because it affects millions of people worldwide. Whether you’re newly diagnosed, supporting a loved one, or just curious, knowing the differences between Type 1 and Type 2 diabetes can make all the difference. Let’s dive into what sets these two types apart and how you can manage them effectively.
What is Diabetes?
Diabetes is a chronic condition that affects how your body processes blood sugar (glucose). Glucose is vital for energy, but when it’s not regulated correctly, it can lead to serious health issues. There are two primary types of diabetes: Type 1 and Type 2.
Type 1 Diabetes
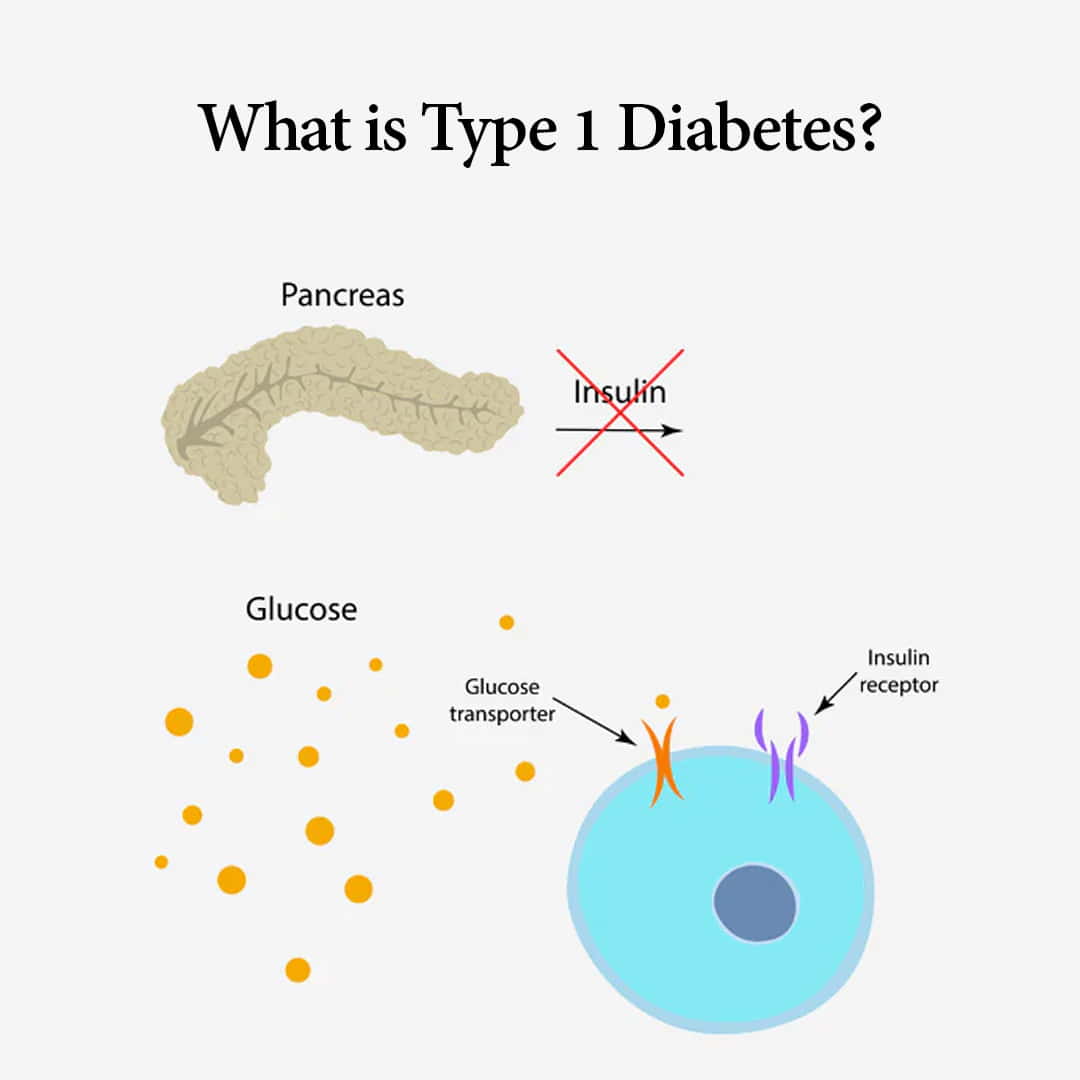
What is Type 1 Diabetes?
Type 1 diabetes, often referred to as juvenile diabetes, is an autoimmune condition where the body’s immune system attacks and destroys insulin-producing cells in the pancreas. This means the body can no longer produce insulin, a hormone necessary to regulate blood glucose levels.
Causes of Type 1 Diabetes
The exact cause of Type 1 diabetes is unknown, but it is believed to involve a combination of genetic and environmental factors. Unlike Type 2, lifestyle factors do not play a significant role in its development.
Symptoms and Diagnosis
Symptoms of Type 1 diabetes often appear suddenly and can include:
- Extreme thirst and hunger
- Frequent urination
- Unintended weight loss
- Fatigue
- Blurred vision
Diagnosis usually involves blood tests to measure blood sugar levels and the presence of autoantibodies indicative of an autoimmune attack on the pancreas.
Treatment and Management
Managing Type 1 diabetes requires regular monitoring of blood sugar levels and lifelong insulin therapy. This can be administered through injections or an insulin pump. Diet, exercise, and monitoring blood sugar are essential to managing this condition.
Type 2 Diabetes
What is Type 2 Diabetes?
Type 2 diabetes is the most common form of diabetes, typically developing in adults over the age of 45, though it’s becoming increasingly prevalent in younger populations. In Type 2 diabetes, the body either becomes resistant to insulin or doesn’t produce enough insulin.
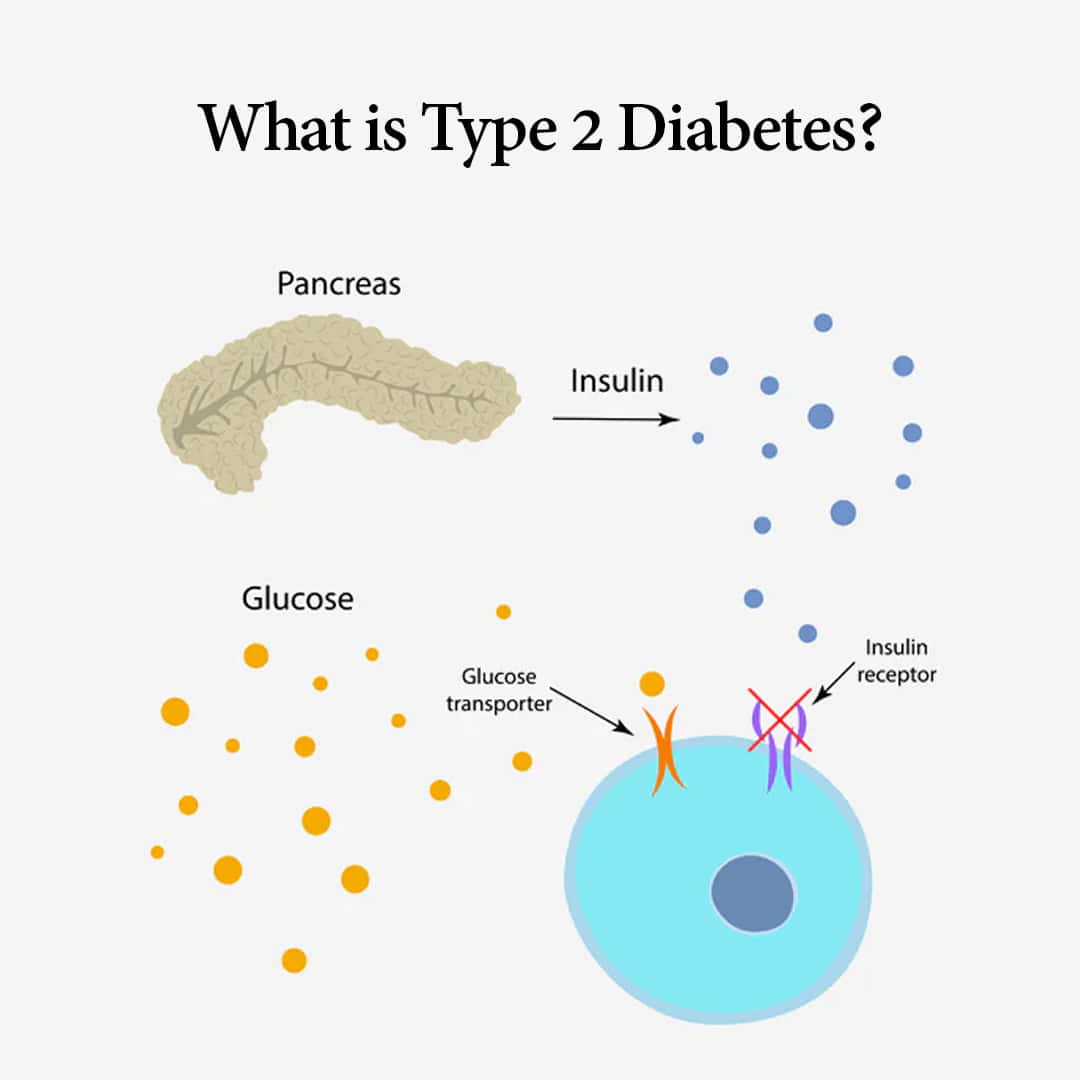
Causes of Type 2 Diabetes
Lifestyle factors and genetics heavily influence the development of Type 2 diabetes. Risk factors include:
- Obesity
- Sedentary lifestyle
- Poor diet
- Family history of diabetes
Symptoms and Diagnosis
Symptoms of Type 2 diabetes often develop gradually and may include:
- Increased thirst and hunger
- Frequent urination
- Fatigue
- Blurred vision
- Slow-healing sores
Diagnosis typically involves blood tests that measure average blood sugar levels over the past two to three months (A1C test) or fasting blood glucose tests.
Treatment and Management
Treatment for Type 2 diabetes focuses on lifestyle changes such as diet and exercise, often combined with medications to improve blood sugar control. In some cases, insulin therapy may be necessary.
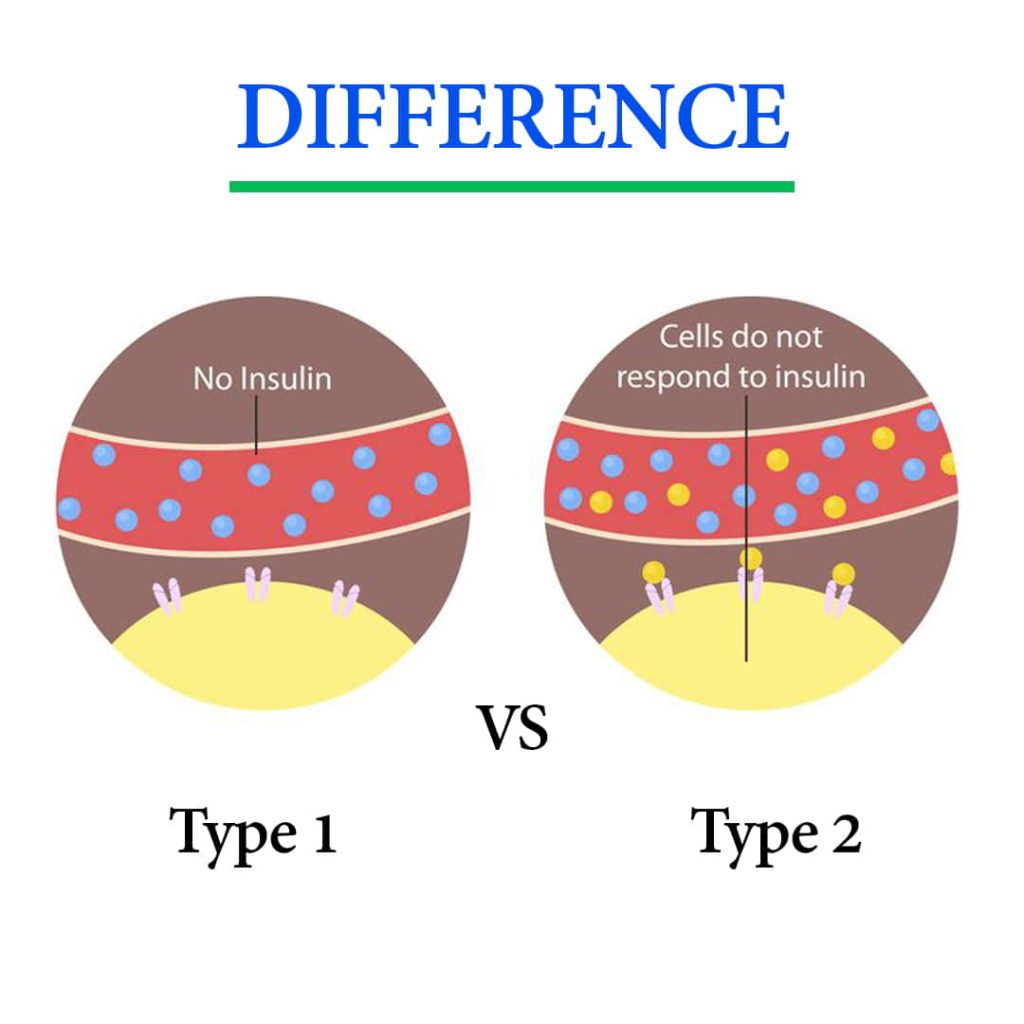
Critical Differences Between Type 1 and Type 2 Diabetes
Age of Onset
- Type 1: Typically diagnosed in children and young adults but can occur at any age.
- Type 2: More commonly diagnosed in adults over 45 but increasingly found in younger people due to rising obesity rates.
Causes and Risk Factors
- Type 1: Primarily due to an autoimmune response. Not linked to lifestyle factors.
- Type 2: Strongly associated with obesity, inactivity, and poor diet. Genetics also plays a significant role.
Symptoms
While both types share some common symptoms, Type 1 symptoms usually appear suddenly and are more severe at onset, whereas Type 2 symptoms develop slowly over time.
Treatment Approaches
- Type 1: Requires insulin therapy and regular blood sugar monitoring.
- Type 2: Managed with lifestyle changes, medications, and sometimes insulin therapy.
Lifestyle Impact
- Type 1: Intensive and lifelong management is required from an early age.
- Type 2: Management often includes significant lifestyle adjustments, especially if diagnosed later in life.
Risk Factors and Prevention
Risk Factors for Type 1 Diabetes
- Family history of Type 1 diabetes
- Genetic predisposition
- Environmental triggers (viruses, early diet)
Risk Factors for Type 2 Diabetes
- Obesity
- Sedentary lifestyle
- Poor diet
- Age (45+)
- Family history of diabetes
- Ethnic background (higher risk in African American, Hispanic, Native American, and Asian populations)
Preventive Measures for Type 1 and Type 2 Diabetes
- Type 1: Currently, there are no known ways to prevent Type 1 diabetes.
- Type 2: Prevention strategies include maintaining a healthy weight, regular physical activity, and a balanced diet low in refined sugars and fats.
Complications of Diabetes
Common Complications of Diabetes
- Cardiovascular disease
- Kidney damage (nephropathy)
- Nerve damage (neuropathy)
- Eye damage (retinopathy)
- Foot problems (ulcers and infections)
How to Prevent Complications
Managing blood sugar levels through medication, diet, and exercise is crucial. Regular check-ups with healthcare providers to monitor for early signs of complications can also help mitigate risks.
Living with Diabetes
Daily Management Tips
- Monitor blood sugar levels regularly
- Follow a diabetes-friendly diet
- Stay active
- Take medications as prescribed
- Attend regular medical check-ups
Diet and Exercise Recommendations
Focus on a balanced diet rich in vegetables, whole grains, lean proteins, and healthy fats. Regular exercise, such as walking or cycling, helps manage blood sugar and overall health.
Mental Health and Diabetes
Managing diabetes can be stressful. It’s important to address mental health through support groups, counseling, or stress-reducing activities like yoga or meditation.
Technological Advances in Diabetes Management
Innovations in Monitoring and Treatment
- Continuous glucose monitors (CGMs)
- Insulin pumps and smart pens
- Artificial pancreas systems
- Telemedicine and mobile health apps
The Future of Diabetes Care
Emerging research on gene therapy, beta cell regeneration, and advanced drug therapies holds promise for more effective diabetes management and potential cures.
Diabetes Myths and Facts
Common Misconceptions
- “Overeating sugar causes diabetes.”
- “People with diabetes can’t eat carbs.“
- “Type 2 diabetes isn’t serious.”
Clarifying the Facts
- Fact: Diabetes is more about how the body processes glucose, not just sugar intake.
- Fact: Carbohydrates are essential but need to be managed appropriately.
- Fact: Both types of diabetes require careful management and can lead to severe complications if untreated.
Case Studies
Real-Life Experiences of Individuals with Type 1 Diabetes
Story of a young athlete managing Type 1 diabetes while excelling in sports.
Real-Life Experiences of Individuals with Type 2 Diabetes
Journey of an older adult reversing Type 2 diabetes through lifestyle changes and dedication.
Support and Resources
Organizations and Communities for Diabetes Support
- American Diabetes Association (ADA)
- Juvenile Diabetes Research Foundation (JDRF)
- Diabetes UK
Educational Resources for Further Learning
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
- Mayo Clinic
- Centers for Disease Control and Prevention (CDC)
Conclusion
Understanding the differences between Type 1 and Type 2 diabetes is essential for effective management and support. Both require lifelong care and attention, but individuals can lead entire and active lives with the proper knowledge and resources. Stay informed, stay proactive, and don’t hesitate to seek support when needed.
FAQs
1. Can Type 1 Diabetes Turn into Type 2?
No, Type 1 and Type 2 diabetes are distinct conditions. Type 1 is an autoimmune disease, while Type 2 is often related to lifestyle factors.
2. Is Type 2 Diabetes More Serious Than Type 1?
Both types are severe and require management. The complications and health risks can be significant if neither type is managed appropriately.
3. Can Diet Alone Manage Type 2 Diabetes?
Diet is crucial in managing Type 2 diabetes, but many individuals also require medication or insulin therapy to control their blood sugar levels effectively.
4. What is Prediabetes?
Prediabetes is a condition where blood sugar levels are higher than usual but not yet high enough to be classified as Type 2 diabetes. It is a warning sign that diabetes could develop if lifestyle changes are not made.
5. How Can You Support Someone with Diabetes?
Offer emotional support, encourage healthy habits, and educate yourself about the condition to provide informed assistance.