Pollen allergy, also known as hay fever or allergic rhinitis, is a common condition where your immune system overreacts to pollen grains released by plants. These tiny particles, meant for plant reproduction, are seen by your body as harmful invaders. As a result, your immune system launches an attack, causing sneezing, watery eyes, and other allergic symptoms. This condition can be seasonal or year-round, depending on the type of pollen and individual sensitivities.
How Pollen Triggers Allergic Reactions
When pollen enters the nose or eyes, the immune system of allergic individuals identifies it as a threat. In response, it releases chemicals like histamine that cause inflammation and allergy symptoms. This immune response is what leads to sneezing, itching, and nasal congestion. The reaction is more intense when pollen counts are high, especially during spring and fall.
Common Types of Pollen-Causing Allergy
Not all pollen triggers allergic reactions. The most common offenders are:
- Tree Pollen (oak, birch, cedar)
- Grass Pollen (timothy, Bermuda, rye)
- Weed Pollen (ragweed, sagebrush, pigweed)
These types are light and easily spread by the wind, making them more likely to be inhaled.
Who Is Most at Risk of Pollen Allergy?
Anyone can develop a pollen allergy, but it’s more common in:
- People with a family history of allergies
- Individuals with asthma or eczema
- Children and young adults
- People exposed to high pollen levels regularly
Causes of Pollen Allergy
Environmental Triggers
Living in areas with high pollen-producing plants increases your exposure. Urban areas with lots of trees and green spaces can be hotbeds of pollen activity.
Genetic Predisposition
If one or both of your parents suffer from allergies, your chances of developing a pollen allergy increase significantly. Genetics plays a key role in allergic sensitivity.
Immune System Malfunction
In people with pollen allergy, the immune system mistakenly identifies pollen as a harmful substance and triggers an unnecessary reaction, even when there’s no real threat.
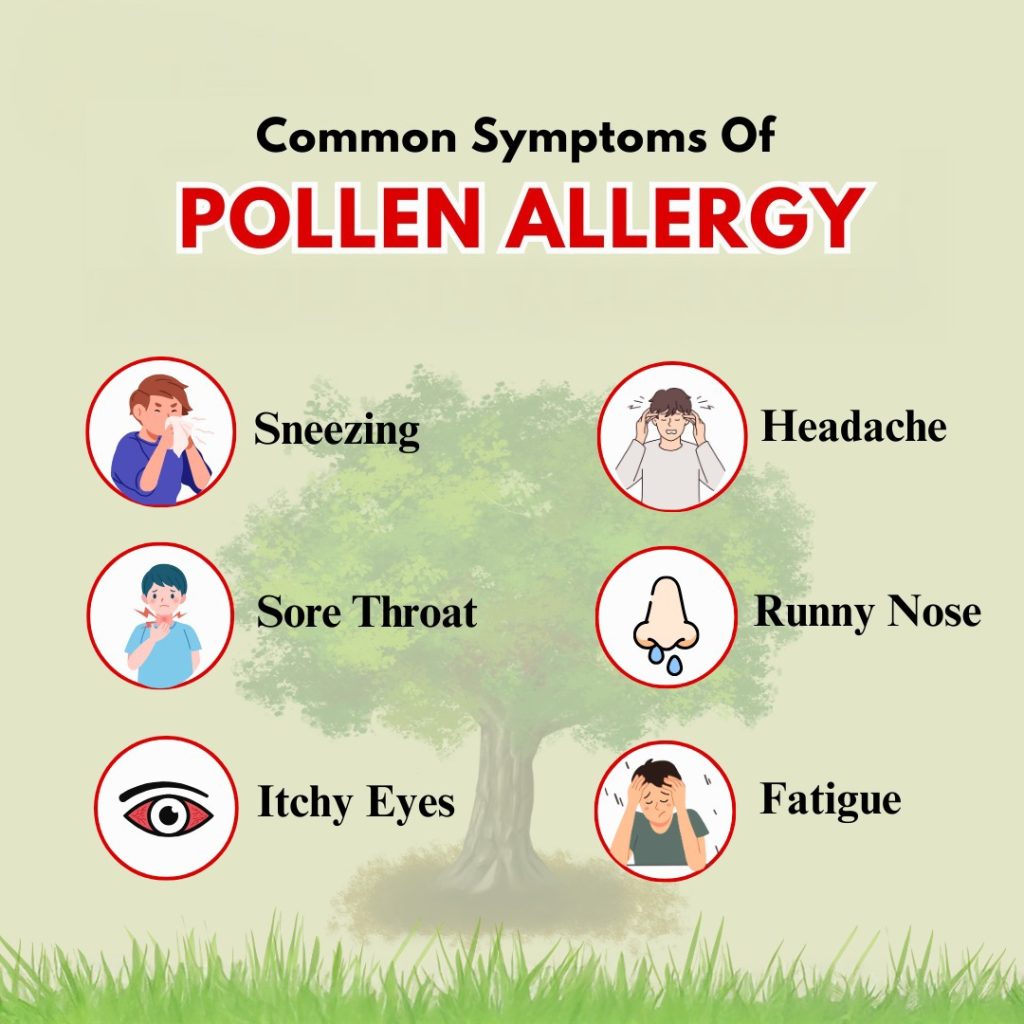
Symptoms of Pollen Allergy
Sneezing and Runny Nose
One of the earliest and most common symptoms, sneezing, occurs as the body tries to expel the allergen. A persistent runny nose usually follows.
Nasal Congestion and Postnasal Drip
Swollen nasal passages block airflow, leading to congestion. Postnasal drip occurs when excess mucus runs down the back of the throat, causing discomfort and coughing.
Itchy Eyes, Nose, and Throat
Itchiness is a hallmark sign of allergies. The histamine released causes nerve irritation, resulting in itchy sensations.
Fatigue and Sleep Disruption
Constant nasal issues and inflammation can lead to poor sleep quality, daytime fatigue, and difficulty concentrating.
Diagnosing Pollen Allergy
Skin Prick Test
In this test, small amounts of pollen allergens are introduced into the skin using a tiny needle. If a raised bump appears, you’re allergic to that type of pollen.
Blood Test for IgE Antibodies
A lab test checks for the presence of IgE antibodies, which are elevated in people with allergies. This helps identify specific allergen sensitivities.
Keeping a Symptom Diary
Recording your symptoms daily can help your doctor identify patterns and link them to pollen levels in your area.
Seasonal vs. Perennial Pollen Allergy
Key Differences
- Seasonal Allergies occur during specific times of the year (spring and fall).
- Perennial allergies happen year-round and may involve indoor allergens like dust mites.
How Seasons Affect Pollen Levels
- Spring: Tree pollen peaks
- Summer: Grass pollen dominates
- Fall: Ragweed pollen surges
Understanding these cycles helps with preparation and prevention.
Understanding the Pollen Count
What Is a Pollen Count?
Pollen count refers to the concentration of pollen grains in the air. It’s usually measured in grains per cubic meter and reported daily in weather forecasts.
How to Monitor Pollen Forecasts
Websites and apps like Weather.com, Pollen.com, and local meteorological services provide daily updates. Watching these can help you plan your day better.
Natural Remedies for Pollen Allergy
Nasal Irrigation with Saline
Nasal irrigation helps flush out pollen, dust, and other allergens from your nasal passages. Using a saline solution with a neti pot or squeeze bottle provides immediate relief by clearing mucus and reducing inflammation. It’s safe for daily use during allergy seasons and can be more effective than some over-the-counter medications when done consistently.
Herbal Supplements
Some herbs have natural antihistamine and anti-inflammatory properties. Popular supplements include:
- Butterbur: It may reduce nasal symptoms in a way similar to antihistamines.
- Stinging Nettle: Known to reduce histamine levels.
- Quercetin: A flavonoid found in onions and apples that is helpful in stabilizing mast cells.
Always consult your doctor before adding supplements to your routine.
Honey and Local Pollen
Some believe that small amounts of local honey help build tolerance to regional pollen, although scientific evidence is limited. If nothing else, honey can soothe irritated throats and act as a natural cough suppressant.
Medical Treatments
Antihistamines
These medications block the action of histamine, a chemical released during an allergic reaction. Popular options include:
- Loratadine (Claritin)
- Cetirizine (Zyrtec)
- Fexofenadine (Allegra)
They reduce sneezing, runny nose, and itching with minimal drowsiness.
Decongestants
Decongestants shrink swollen nasal passages and relieve congestion. They are available as pills or nasal sprays (e.g., pseudoephedrine or oxymetazoline). Note: nasal sprays should not be used for more than 3 consecutive days.
Corticosteroid Nasal Sprays
These are effective in reducing inflammation and long-term allergy symptoms. Common sprays include:
- Fluticasone (Flonase)
- Mometasone (Nasonex)
They work best when used regularly and preventively during high pollen seasons.
Immunotherapy (Allergy Shots)
For persistent and severe allergies, immunotherapy may be recommended. This involves regular injections of small amounts of allergens to desensitize your immune system over time. It’s a long-term solution that can reduce or even eliminate allergic reactions.
Lifestyle Tips to Reduce Exposure
Indoor Air Quality
Using HEPA filters in your air conditioners and vacuum cleaners can dramatically reduce indoor pollen exposure. Also, consider using a dehumidifier to keep the air dry, which discourages mold growth and allergen spread.
Cleaning and Dust Reduction
Regularly clean floors, furniture, and curtains. Keep windows closed during high pollen seasons. Shower and change clothes after being outdoors to prevent pollen from spreading around your home.
Wearing Masks Outdoors
Masks like N95s not only protect against viruses but also help filter out airborne allergens, including pollen. This is particularly helpful when doing yard work or walking during high pollen days.
Diet and Pollen Allergy
Anti-Inflammatory Foods
Eating a diet rich in anti-inflammatory foods can help reduce allergic reactions. Try incorporating:
- Omega-3 rich fish (salmon, mackerel)
- Leafy greens
- Turmeric
- Ginger
- Berries
These foods support a healthy immune system and reduce inflammation.
Foods to Avoid
Certain foods can worsen symptoms due to cross-reactivity, especially in people with oral allergy syndrome. These include:
- Apples (if allergic to birch pollen)
- Melons (if allergic to ragweed)
- Bananas and zucchini
Always monitor your body’s reaction after eating raw fruits and vegetables during allergy season.
Home Remedies and DIY Solutions
Steam Inhalation
Steam therapy can help relieve congestion and open up airways. Add a few drops of eucalyptus or peppermint oil to a bowl of hot water, cover your head with a towel, and breathe in the vapors for relief.
Essential Oils for Allergy Relief
Certain essential oils like lavender, eucalyptus, and tea tree oil have anti-inflammatory and antimicrobial properties. You can diffuse them or use them in baths for calming effects. Always dilute properly before skin application.
Pollen Allergy in Children
Symptoms to Watch for
Children may experience:
- Constant sneezing
- Red, watery eyes
- Itchy nose and throat
- Trouble sleeping or concentrating at school
Because they may not express discomfort clearly, parents should observe these signs closely.
Best Treatments for Kids
Children can benefit from:
- Pediatric antihistamines (Claritin, Zyrtec)
- Saline nasal sprays
- Keeping their environment pollen-free
Consult a pediatrician before starting any treatment plan.
Pollen Allergy and Asthma
How They’re Connected
People with asthma often have pollen allergies, too. Pollen can worsen asthma symptoms like wheezing, chest tightness, and shortness of breath.
Managing Both Conditions Together
- Stick to prescribed inhalers and allergy medications
- Monitor pollen forecasts
- Use air purifiers and stay indoors on high pollen days
Combining asthma and allergy treatments often results in better control of both conditions.
When to See a Doctor
Warning Signs of Severe Allergies
- Shortness of breath
- Wheezing
- Facial swelling
- Severe fatigue
These signs may indicate a more serious condition like anaphylaxis or uncontrolled asthma and require immediate attention.
Preparing for Your Appointment
- Keep a diary of your symptoms
- Track exposure patterns
- List medications and supplements you’re using
This will help your doctor diagnose and tailor treatment more effectively.
Pollen Allergy Prevention Tips
Long-Term Lifestyle Changes
- Move to low-pollen areas if symptoms are severe
- Limit outdoor activities during the pollen season
- Practice daily nasal rinses
- Wear sunglasses to protect your eyes
These steps can significantly reduce your risk over time.
Travel Tips for Allergy Sufferers
- Check pollen forecasts at your destination
- Pack your allergy medications
- Choose accommodations with air filtration
Planning is key when traveling with pollen allergies.
Myths About Pollen Allergy
Common Misconceptions
- “You can’t develop allergies as an adult” – Not true; adult-onset allergies are common.
- “Rain eliminates all pollen” – Rain may reduce it briefly, but wind afterward can stir it up again.
Facts That Dispel the Myths
- Allergies can begin at any age.
- Pollen levels vary by time of day and weather conditions.
- Natural remedies can complement, not replace, medical treatment.
FAQs about Pollen Allergy
Can you cure pollen allergy completely?
While there’s no complete cure, treatments like immunotherapy can significantly reduce or eliminate symptoms over time.
How can I tell if it’s a cold or pollen allergy?
Allergies last longer, come with itching and lack fever. Colds are shorter and usually come with body aches and fever.
Is pollen allergy dangerous?
It can lead to complications like sinus infections, asthma attacks, and poor sleep, but it’s rarely life-threatening.
Can I outgrow my pollen allergy?
Some people do outgrow allergies, but it’s not guaranteed. Others may find symptoms worsen over time.
Do air purifiers help with pollen allergies?
Yes, especially those with HEPA filters. They trap pollen and other allergens, improving indoor air quality.
When is the pollen count highest during the day?
Pollen levels are typically highest in the early morning (5 a.m. to 10 a.m.).
Conclusion
Managing pollen allergy requires a combination of awareness, prevention, and effective treatment. By understanding your triggers, monitoring pollen levels, and applying both medical and natural remedies, you can enjoy life with fewer interruptions from allergy symptoms. Whether you’re experiencing mild discomfort or dealing with more severe reactions, taking proactive steps makes all the difference. Remember, with the right tools and support, pollen allergy doesn’t have to control your life.