Diabetes is a group of diseases characterized by high blood sugar (glucose) levels. While there are several types of diabetes, Type 2 diabetes is the most common, accounting for approximately 90-95% of all diabetes cases. Unlike Type 1 diabetes, which is primarily genetic and autoimmune, Type 2 is largely influenced by lifestyle and dietary factors.
Overview of Diabetes
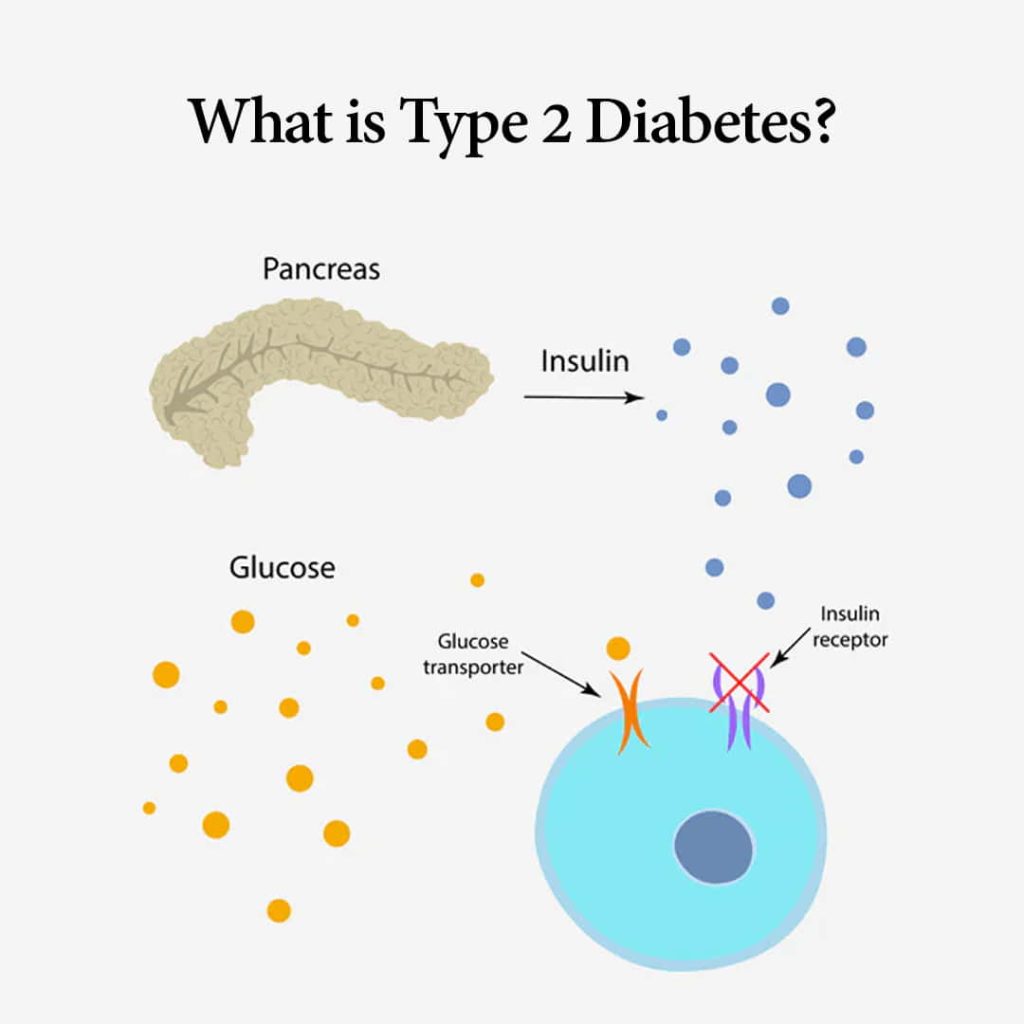
At its core, diabetes involves issues with the body’s ability to produce or use insulin effectively. Insulin is a hormone produced by the pancreas that allows cells to absorb glucose from the bloodstream for energy. In people with diabetes, this process is impaired, leading to elevated blood glucose levels, which can cause a range of health issues over time.
Distinguishing Type 2 from Type 1 Diabetes
Type 1 diabetes is an autoimmune condition where the body attacks insulin-producing cells in the pancreas, leading to little or no insulin production. It usually manifests early in life. In contrast, Type 2 diabetes typically develops in adults, though increasing numbers of children and adolescents are being diagnosed. Type 2 diabetes is characterized by insulin resistance, where the body’s cells do not respond effectively to insulin.
Understanding Type 2 Diabetes
Definition and Mechanism
Type 2 diabetes occurs when the body either resists the effects of insulin or does not produce enough insulin to maintain normal glucose levels. Insulin resistance leads to glucose buildup in the blood instead of being absorbed by the cells, resulting in hyperglycemia. Over time, high blood sugar can damage various organs and systems.
Prevalence and Statistics
Type 2 diabetes is a global health concern. According to the International Diabetes Federation, as of 2021, over 460 million people worldwide live with diabetes, and the majority of these cases are Type 2. The incidence of this disease is rising, especially in low- and middle-income countries, due to urbanization, sedentary lifestyles, and unhealthy diets.
Causes and Risk Factors
Genetic Predisposition
Genetics plays a significant role in the risk of developing Type 2 diabetes. If you have a family history of the disease, your risk increases. Certain ethnic groups, including African Americans, Hispanic/Latino Americans, Native Americans, and some Asian Americans, are also at higher risk.
Lifestyle and Diet
Lifestyle factors are crucial contributors to Type 2 diabetes. A diet high in processed foods, sugary drinks, and unhealthy fats can lead to weight gain and metabolic disturbances that increase the risk of developing the disease.
Obesity and Metabolic Syndrome
Obesity is one of the most significant risk factors for Type 2 diabetes. Excess body fat around the abdomen can lead to insulin resistance. Metabolic syndrome, a cluster of conditions including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels, significantly increases the risk of Type 2 diabetes.
Symptoms of Type 2 Diabetes
Early Signs
In the early stages, Type 2 diabetes might not present noticeable symptoms. Many people go undiagnosed for years. However, some early warning signs include increased thirst, frequent urination, excessive hunger, fatigue, and blurred vision.
Advanced Symptoms
As the disease progresses, symptoms may become more severe. These can include slow-healing sores, frequent infections, darkened skin in areas such as the neck and armpits (acanthosis nigricans), and numbness or tingling in the hands and feet.
Complications
Without proper management, Type 2 diabetes can lead to severe complications. These include heart disease, stroke, kidney damage (nephropathy), eye damage (retinopathy), and nerve damage (neuropathy). The risk of these complications underscores the importance of early detection and consistent management.
Diagnosis of Type 2 Diabetes
Medical Tests
Several tests are used to diagnose Type 2 diabetes. The most common are:
- Fasting Blood Sugar Test: Measures blood glucose after an overnight fast.
- A1C Test: Reflects average blood glucose levels over the past 2-3 months.
- Oral Glucose Tolerance Test (OGTT): Measures blood glucose before and after consuming a sugary drink.
Understanding Blood Sugar Levels
Normal blood sugar levels vary depending on the time of day and the individual’s last meal. Generally, a fasting blood sugar level of less than 100 mg/dL is average; 100-125 mg/dL indicates prediabetes and 126 mg/dL or higher suggests diabetes.
The Role of Insulin in Type 2 Diabetes
Insulin Resistance Explained
In Type 2 diabetes, muscle, fat, and liver cells start resisting or ignoring the insulin signal. This means they don’t take up glucose from the blood as effectively. The pancreas compensates by producing more insulin, but it can’t keep up over time, leading to higher blood sugar levels.
How Insulin Works
Insulin acts like a key, unlocking cells to allow glucose to enter and be used for energy. In Type 2 diabetes, this key is either not produced sufficiently, or the lock (cell receptors) is defective. This leads to glucose staying in the bloodstream, causing high blood sugar levels.
Managing Type 2 Diabetes
Lifestyle Modifications
Management of Type 2 diabetes often starts with lifestyle changes. This includes adopting a healthier diet, increasing physical activity, and losing weight if necessary. These steps can help lower blood sugar levels and improve the body’s sensitivity to insulin.
Importance of Diet
Diet is a cornerstone of diabetes management. Emphasize whole foods, such as fruits, vegetables, whole grains, and lean proteins, and limit processed foods and sugary beverages. Carbohydrate counting and meal planning can also help keep blood sugar levels stable.
Regular Physical Activity
Exercise helps manage weight, improves insulin sensitivity, and lowers blood sugar levels. Aim for at least 150 minutes of moderate aerobic activity per week, such as brisk walking or cycling, combined with strength training exercises.
Medical Treatments for Type 2 Diabetes
Oral Medications
Several classes of oral medications can help manage Type 2 diabetes by improving insulin sensitivity, increasing insulin production, or decreasing liver glucose production. Common types include metformin, sulfonylureas, and DPP-4 inhibitors.
Insulin Therapy
Sometimes, oral medications are insufficient, and insulin therapy may be required. This is more common in advanced stages of the disease when the pancreas can no longer produce adequate insulin.
Emerging Treatments
Research into new treatments for Type 2 diabetes is ongoing. This includes medications that offer improved blood sugar control and treatments that target the underlying causes of the disease. Innovations in diabetes technology, such as continuous glucose monitors and insulin pumps, also provide new ways to manage the condition effectively.
Monitoring and Controlling Blood Sugar Levels
Importance of Monitoring
Regular monitoring of blood sugar levels is crucial for managing Type 2 diabetes. It helps you understand how different foods, activities, and medications affect your blood sugar levels, allowing for more precise control.
Tools and Techniques
Various tools are available for monitoring blood sugar, from traditional finger-stick tests to continuous glucose monitors that provide real-time data. Keeping a log of your readings can help track patterns and make necessary adjustments to your management plan.
Complications Associated with Type 2 Diabetes
Cardiovascular Issues
People with Type 2 diabetes are at increased risk of cardiovascular diseases, including heart attack and stroke. High blood sugar can damage blood vessels and nerves that control the heart.
Neuropathy and Kidney Disease
Diabetic neuropathy can cause pain, tingling, or numbness in the extremities. Kidney disease, or nephropathy, can lead to kidney failure and requires dialysis or a transplant in severe cases.
Eye Problems
Diabetes can lead to various eye problems, including diabetic retinopathy, which can cause blindness. Regular eye exams are essential to catch and treat these issues early.
Preventing Type 2 Diabetes
Lifestyle Changes
Preventing Type 2 diabetes involves adopting a healthy lifestyle. This includes maintaining a balanced diet, staying physically active, and keeping a healthy weight. Avoiding tobacco use and limiting alcohol can also reduce the risk.
Preventive Screenings
Regular screenings for blood sugar levels can identify prediabetes or early diabetes. Early detection allows for lifestyle interventions that can delay or prevent the onset of full-blown Type 2 diabetes.
The Psychological Impact of Type 2 Diabetes
Dealing with Diagnosis
Being diagnosed with Type 2 diabetes can be overwhelming. It’s essential to seek support from healthcare providers, family, and friends to navigate the emotional aspects of the disease.
Mental Health Considerations
Living with a chronic condition like Type 2 diabetes can lead to stress, anxiety, and depression. Addressing these issues through counseling, support groups, or mental health professionals is essential.
Support Systems and Resources
Healthcare Providers
Your healthcare team plays a vital role in managing Type 2 diabetes. This includes your primary care physician, endocrinologist, dietitian, and diabetes educator.
Diabetes Education Programs
Education programs can provide valuable information on managing diabetes, from understanding your condition to learning about diet and exercise strategies.
Living Well with Type 2 Diabetes
Personal Stories and Testimonials
Hearing from others with Type 2 diabetes can be inspiring and provide practical tips for managing the condition. Personal stories can highlight the resilience and adaptability required to live well with diabetes.
Community and Support Groups
Joining a diabetes support group can offer emotional support and practical advice. Connecting with others facing similar challenges can make a significant difference in managing the disease.
Future Directions in Diabetes Research
Advances in Treatment
Research into new diabetes treatments is ongoing. Future therapies may offer better blood sugar control, fewer side effects, and treatments that address the root causes of Type 2 diabetes.
Ongoing Research and Innovations
Innovations in diabetes care, such as new medications, advanced monitoring technologies, and potential cures, are on the horizon. Staying informed about these developments can help those with Type 2 diabetes manage their condition more effectively.
Conclusion
Type 2 diabetes is a manageable condition, but it requires a comprehensive approach involving lifestyle changes, regular monitoring, and sometimes medication. Understanding the disease, its causes, and how to manage it effectively can empower individuals to lead healthy, active lives. By staying informed and proactive, you can take control of your health and minimize the impact of Type 2 diabetes.
FAQs
- What is the leading cause of Type 2 diabetes?
- Type 2 diabetes is primarily caused by insulin resistance and the body’s inability to use insulin effectively. Factors like genetics, obesity, and a sedentary lifestyle significantly contribute to the development of the disease.
- Can Type 2 diabetes be reversed?
- While there is no cure for Type 2 diabetes, it can be managed effectively. People can sometimes achieve remission through significant lifestyle changes, such as weight loss, diet, and increased physical activity.
- What foods should I avoid if I have Type 2 diabetes?
- It’s best to avoid foods high in sugar, processed foods, and those with high glycemic indices, such as white bread, sugary drinks, and pastries. Focus on whole foods, including vegetables, lean proteins, and whole grains.
- How often should I monitor my blood sugar levels?
- The frequency of blood sugar monitoring depends on your treatment plan. People on insulin may need to check several times daily, while those managing diabetes with diet and oral medications might check less frequently. Consult your healthcare provider for personalized advice.
- Can exercise help manage Type 2 diabetes?
- Absolutely! Regular physical activity helps improve insulin sensitivity, lowers blood sugar levels, and aids in weight management. For the best results, combine aerobic exercises with strength training.